Our Blog
A Glossary of the Massage Therapy Profession
Demystify massage therapy organizations. Learn about major associations and their roles. ...more
Blog
April 30, 2024•3 min read

Healwell is seeding change!
Healwell's new logo is based on dandelion imagery which, I think you’ll agree, is deeply fitting. ...more
Blog
January 25, 2024•3 min read
The Top Five Things You Should Know About Hospital-Based Massage Therapy
Massage therapists are more than “nice to have.” ...more
Blog
September 08, 2023•7 min read
Disparity is Death
None of us know the names of the Black women with breast cancer who make up the “40% more” deaths than their white counterparts every year. This is partly by design. ...more
Blog
August 03, 2023•5 min read

Connection
It's no surprise to you that humans are social creatures. We crave connection and the feeling of belonging. ...more
Blog
July 24, 2023•2 min read
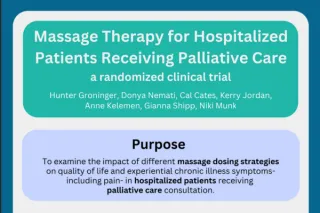
Healwell Dosing Study Infographic
Corey Rivera created this excellent infographic to help you understand Healwell's latest dosing study. ...more
Blog
July 01, 2023•0 min read

Three Reasons You Should Read Research
Corey Rivera shares three reasons you should read research... and three reasons why you might not. ...more
Blog
June 27, 2023•2 min read

Ways to Give
You already know that Healwell does important work. What you might not know is that all that work is made possible by generous people like you. ...more
Blog
May 08, 2023•4 min read

Have you ever gone to a funeral...
Have you ever gone to a funeral, and the deceased wasn't there? ...more
Blog
April 14, 2023•3 min read

Thank You for Listening
Every word and action make an impact. ...more
Blog
February 15, 2023•1 min read

Living with Juvenile Arthritis
July is Juvenile Arthritis Awareness month for recognizing the 300,000 or so children in the U.S. with the disease. ...more
Blog
July 04, 2022•3 min read
Strange Bedfellows
Massage therapy has a sex problem. We don’t like to talk about it. ...more
Blog
June 20, 2022•6 min read

Trusting (and Supporting) Nurses
I trust nurses. Doctors? Sure, they’re fine, they diagnose and treat. But nurses do the hardest work – the care work – without the accolades or the pay that doctors receive. ...more
Blog
May 20, 2022•2 min read

Conscious Discomfort
I have two experiences that are coming together in my life in a very interesting way... ...more
Blog
April 27, 2022•2 min read

Out of the Community and Into the Fire
Can social media be useful in the fight for social justice, or are you just screaming into the void? ...more
Blog
March 31, 2022•1 min read
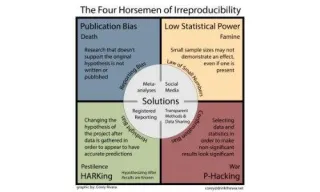
Flawed Research
Cal's most recent column for Massage & Bodywork Magazine explores four reasons why it's difficult to conduct a proper study. ...more
Blog
March 14, 2022•2 min read
Apology and Forgiveness
Apology and forgiveness. So simple, right? Then why do we all find it so difficult? ...more
Blog
March 04, 2022•1 min read

Social Justice Adventuring Party
The term Social Justice Warrior is often used to refer to people who lean left, liberal or progressive, believe in fairness and generally live in a way that makes it clear that they’re not down with t... ...more
Blog
February 24, 2022•5 min read

More Than One Way
There is more than one way to fight. More than one way to change the future. There has to be. ...more
Blog
February 09, 2022•4 min read
Let's Walk the Walk Before We Talk the Talk
Healthcare professionals (and everyone) need to have more and better conversations about end of life choices and advanced care plans. ...more
Blog
February 01, 2022•1 min read

When Massage Quits You: The Tangible
Being a massage therapist is a rough gig... Among the things that could be under our control, there is a quietly looming monster that patiently waits: disability. ...more
Blog
January 22, 2022•3 min read

When Massage Quits You: The Intangible
What happens when you can’t massage anymore? This is the first of a two-part description on the decline of my ability to perform massage. ...more
Blog
January 15, 2022•4 min read
Telling the Truth
Cal's column for Massage & Bodywork Magazine explores ways that massage therapists can stop being purveyors of misinformation. ...more
Blog
January 07, 2022•1 min read
Real Self-Care
“I do not make resolutions. Winter is not the time to suddenly stop eating.” ~Me on facebook, every year since 2017 ...more
Blog
January 03, 2022•1 min read

Independence
There are so many moments when, if I am listening, I have my every assumption challenged. ...more
Blog
December 15, 2021•2 min read
Searching for Joy
Luckily, rebellions aren’t about what they want us to be, they’re about what we want to create. Sometimes the most defiant acts are those of joy, happiness, and community. ...more
Blog
December 01, 2021•2 min read
How to be Wrong
Massage uses ostriching as a default response to being wrong. A profession that wants to be taken seriously as healthcare should not act this way. ...more
Blog
November 16, 2021•3 min read

Don’t Let Your COVID Guard Down
In this edition of their column for Massage & Bodywork Magazine, Cal warns, "If you’re feeling bored or finding yourself rolling your eyes at “yet another COVID story,” snap out of it. ...more
Blog
November 08, 2021•1 min read

Seeing Past Our Hands
In this column for Massage & Bodywork Magazine, Cal explores measuring the value of the practitioner, not the modality. ...more
Blog
September 07, 2021•1 min read

Harmful Stories
Cal's column for Massage & Bodywork Magazine tackles the stories we tell about health and explores how to dismantle our assumptions. ...more
Blog
July 02, 2021•1 min read

Resources: The Worst Things (Part 2)
Follow-up to "The Worst Things (Part 2)." Resources and recommendations to combat the silo-ing and imagined hierarchy within the massage therapy profession. ...more
Blog
April 16, 2021•2 min read

The Worst Things (Part 2)
This week, we consider the issue of silos and what can reasonably be called in-fighting. ...more
Blog
April 12, 2021•3 min read
Resources: The Worst Things (Part 1)
Follow-up to "The Worst Things (Part 1)." Resources to support self-exploration and elevation of the practice that's happening right under your own hands. ...more
Blog
April 09, 2021•1 min read

The Worst Things (Part 1)
Healwell’s post regarding the social media response to the Atlanta murders that took place at three spas inspired lots of dialogue. ...more
Blog
April 05, 2021•4 min read

Do No Harm
Yesterday morning, nine people were shot in Atlanta at what are being referred to as “massage parlors;” eight of these people were shot fatally. Six of them were Asian women. ...more
Blog
March 18, 2021•5 min read

A New Course
As the Education Director for Healwell, I spend a lot of time in gratitude... Today, I want to talk to the students. ...more
Blog
January 12, 2021•6 min read

Show Up with Healwell
Healwell is now a C-TAC member and we’re really looking forward to attending the upcoming annual C-TAC Summit: Improving Lives by Facing Systemic Injustice, October 28-30, 2020. ...more
Blog
September 14, 2020•3 min read

The Time Has Come
As many of you know, Healwell recently ended its affiliation with Amazon’s “Smile” program. We have heard from some of you and we are deeply sorry that our message did not land as we intended. ...more
Blog
August 28, 2020•4 min read

Being Vulnerable
When I began my training in palliative and end-of-life care, I watched peers laugh and roll their eyes about the inevitable question, “How can you do that kind of work?” ...more
Blog
August 17, 2020•3 min read

Massage Isn't Normal
Wednesday morning I woke up feeling off, just a little tired. It was easy to think I just didn’t have enough sleep. ...more
Blog
July 23, 2020•3 min read

Wanna Help Healwell Get a Seat at the Table?
Do you know about C-TAC? Chances are good that you don’t. ...more
Blog
July 10, 2020•2 min read

Happy-ish Anniversary, Healwell
Healwell turns 10 this week. It’s an anniversary that is much sadder than I would have envisioned... ...more
Blog
June 11, 2020•8 min read

We Are Not Exempt
In the time since early March, we have been brought face-to-face with two serious diseases. One, COVID-19, is spread through droplets. The other, racism, is spread through ignorance and fear. ...more
Blog
June 08, 2020•9 min read

New Guidelines Are Not Too Shabby
FSMTB convened a task force a few weeks ago to put their giant-sized brains together to outline some real guidelines for massage therapists practicing in a variety of settings for safe practice during... ...more
Blog
May 21, 2020•6 min read
An Open Letter to Massage Therapy Consumers
I have been a massage therapist since 2005. If, in pre-COVID-19 times, you were a massage therapy consumer, thank you. ...more
Blog
May 15, 2020•4 min read

Am I covered? Massage therapy, insurance and COVID-19
At Healwell, we have gotten a number of questions from therapists all over the US asking if their liability insurance "covers" them in the event that they get COVID-19 or one of their clients gets COV... ...more
Blog
May 11, 2020•4 min read
The Hangover
It’s hard to hold the hot potato, friends. At Healwell, we expect to continue to do it for a while longer. ...more
Blog
May 10, 2020•6 min read
Worst. Game. Ever.
If another AMTA chapter president calls or emails me for advice and love, I’m going to reach out to National for alimony. ...more
Blog
May 04, 2020•8 min read

Back to Practice
Healwell has been watching our profession divide along the same rancorous political lines as our country. It doesn't have to do that. ...more
Blog
April 24, 2020•4 min read
Your governor is not a massage therapist.
Hello, my massage therapist friends. This is so, so hard. ...more
Blog
April 21, 2020•2 min read
Comfort and Safety
Man, I miss my clients. I hope they miss me. The people I touch are a huge part of my life and even of who I am. ...more
Blog
March 23, 2020•5 min read

Last Call: You Actually Do Have to Go Home. You Can't Stay Here.
Hello, my dearest fellow humans. This is quite a situation in which we find ourselves, isn’t it? ...more
Blog
March 18, 2020•3 min read

I Don't Care About Your Modalities
I am an educated professional. I worked hard to get my license, and I seek out quality continuing education every year... ...more
Blog
December 10, 2019•4 min read

Your Hands Are Great. Who Cares?
“Hands are pretty damn good…and? We [massage therapists] need to be more than that for people.” ...more
Blog
June 17, 2019•2 min read

The Way Forward is Together - Part One
A bill has been introduced in Maine, HB 0255, “An Act To Define Licensed Massage Therapists as Health Care Practitioners...” ...more
Blog
February 14, 2019•4 min read

Making Sausages: Behind the Scenes at the ICM
This month I am embarking on a new and slightly terrifying adventure — I am hosting Healwell’s new webinar series, the Interdisciplinary Clan of Mystery. ...more
Blog
September 16, 2018•3 min read

Meet the team! Katherine LaVelle, Healwell Board Member
Meet Katherine LaVelle, one of the rock-star members of our Board of Directors! ...more
Blog
May 24, 2018•3 min read
Magical Thinking
She looks stunned, mystified. She looks like she has just seen the Statue of Liberty disappear. She looks like she has been touched by magic. ...more
Blog
April 15, 2018•4 min read
An Open Letter to the Massage Therapy Profession: Massage Envy is Our Fault
If “one incident is too many,” then what exactly is 200? That’s my question to Massage Envy... ...more
Blog
December 27, 2017•5 min read
Connect With Us:

Contact Us:
4201 Wilson Blvd. #110-341
Arlington, VA 22203
2024 Healwell | All Rights Reserved
created with Bold Lucidity